Soft & Flexible
Tracoe Silcosoft

A child’s anatomical structures are highly sensitive and at risk of damage from manipulation and pressure. A child’s trachea is relatively narrow and very soft and therefore, small changes can have a big impact. A flexible, kink-resistant but soft tube is gentle on the tracheal mucosa and the stoma itself.6
The Tracoe Silcosoft tracheostomy tube is a soft, flexible silicone tube for neonates, infants and children. They are offered in both a water-filled cuffed and cuffless variations and with or without proximal extension.
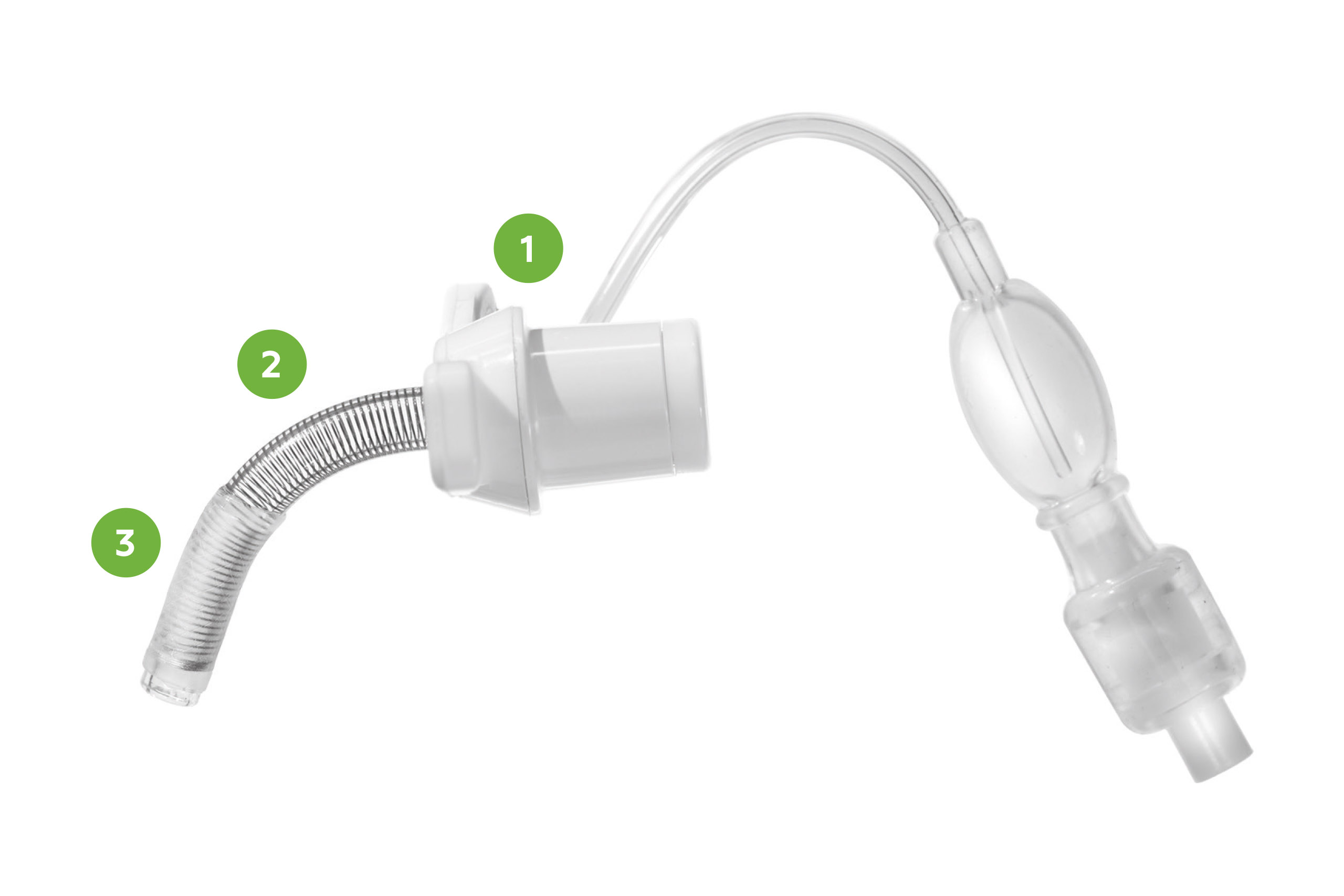
1. Slightly curved neck flange with specially reinforced eyelets
2. Spiral reinforced tube, radiopaque (allows to check position)
3. The cuff is close and tight to the tube in deflated state
The tubes are available in neonatal length (30-36 mm) in sizes from 2.5 mm to 4.0 mm (inner diameter) for neonates and infants, and in pediatric length (38–46 mm) in sizes 2.5 mm to 5.5 mm for children and young people.
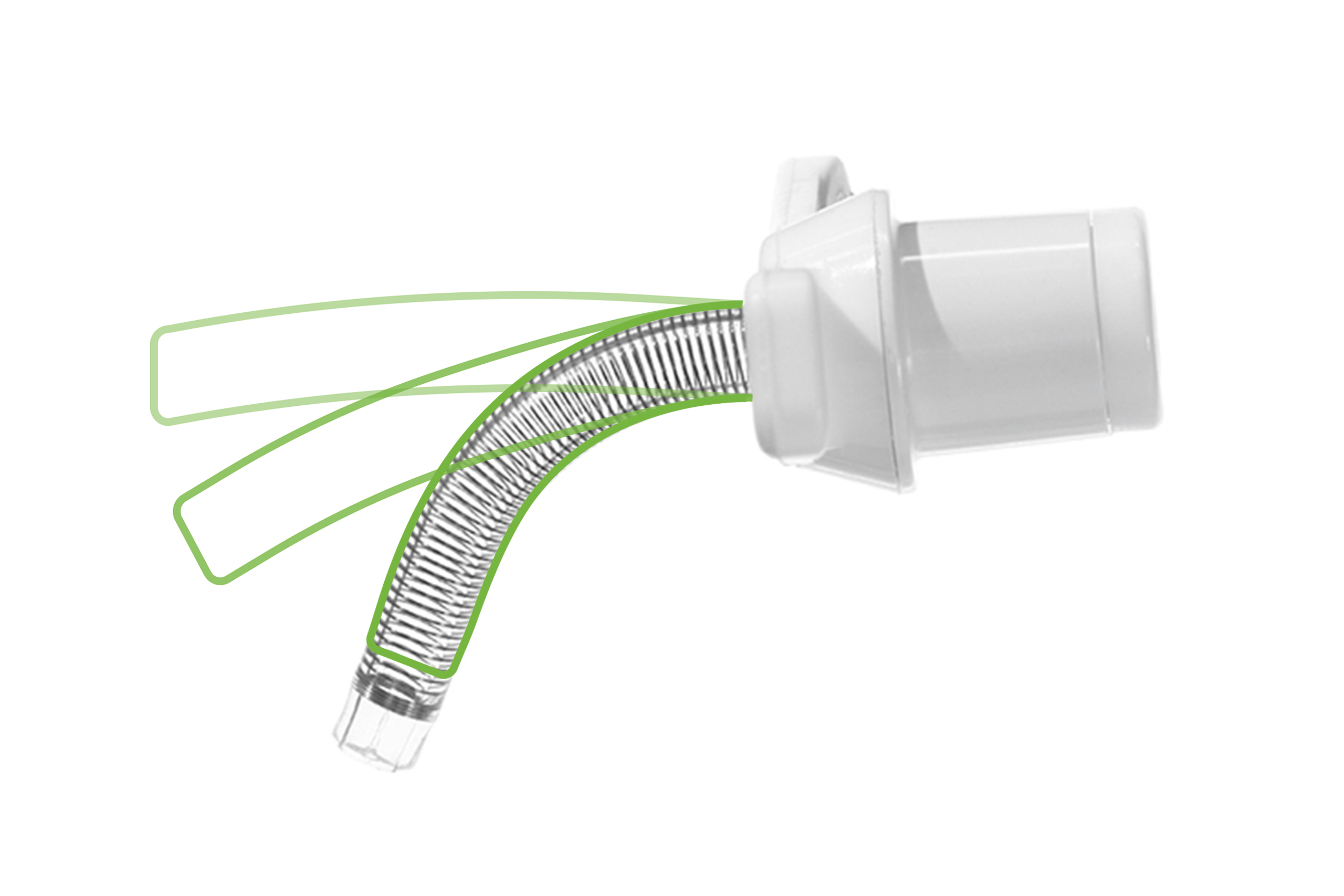
Spiral Reinforced
The Tracoe Silcosoft tracheostomy tube has a spiral reinforcement embedded in the tube wall. The spiral is made from nitinol and therefore all Silcosoft tubes are MR conditional. The tight spiral winding ensures it retains its shape. The spiral winding ends before the end of the tube, which enables a soft tip.
Tracoe Water-Filled (H2O) Cuff
A cuff serves as a seal to minimize the passage of aspirated food, saliva and/or gastric contents into the lower respiratory tract as well as optimize pressures during ventilation.31 The Tracoe H2O cuff must be filled with sterile water. Filling with other liquids, for example, saline or glucose may result in damage to the cuff.25 When the cuff is deflated, it is close and tight to the tracheostomy tube. The cuff inflation line is integrated into the material of the tube wall, which minimizes the risk of potential trauma or damage to the vulnerable pediatric airway mucosa.6,7,32
Silcosoft cuff management
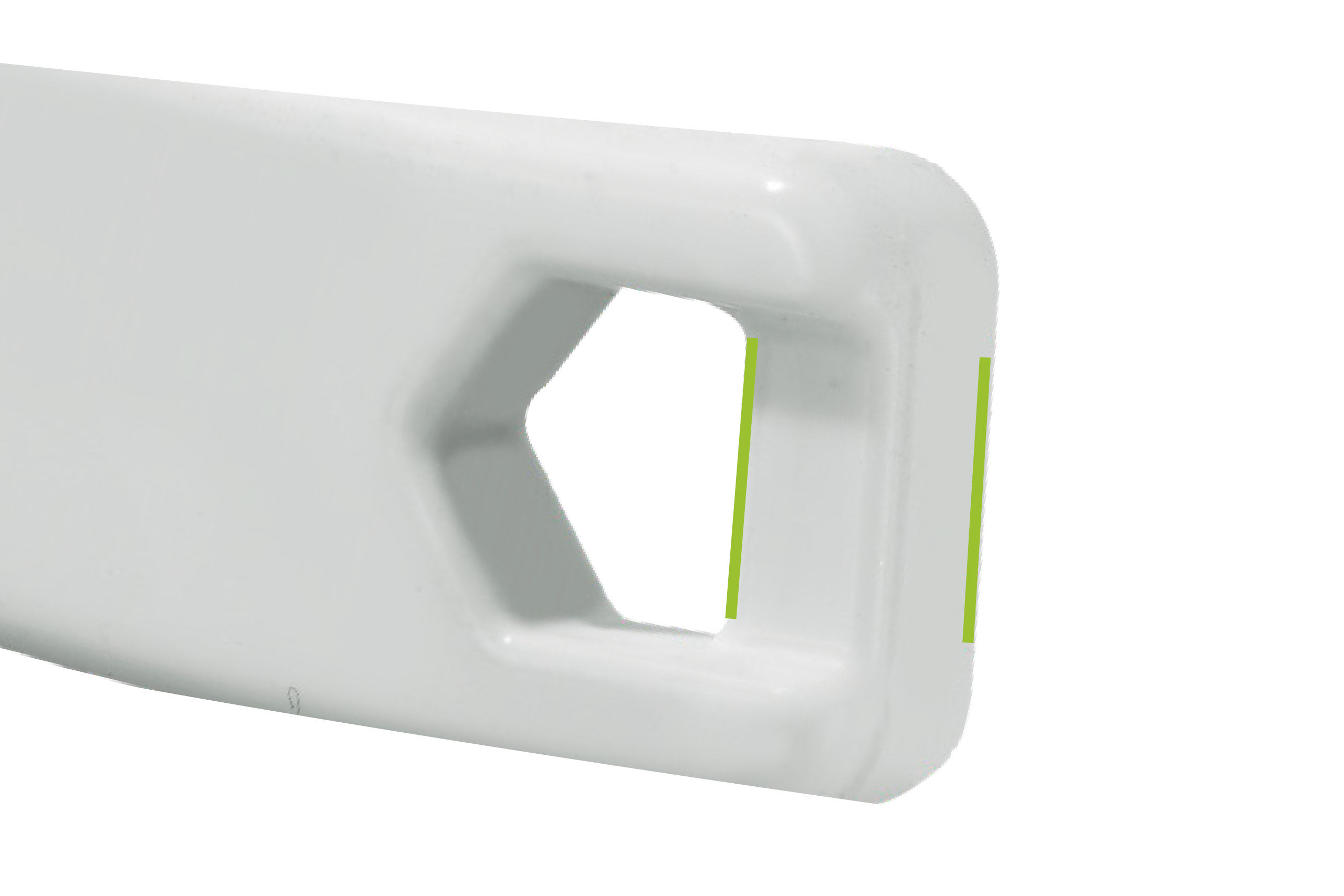
Specially Reinforced Eyelets
Tracoe Silcosoft has a slightly curved neck flange with specially reinforced eyelets. These reinforced eyelets aid confidence particularly when used with hook-and-loop fastener neckbands. An additional feature includes inlets on the underside of the eyelets that allow the neckband to be recessed.
Length Variants
As a child or young individual undergoes growth and development, the dimensions of a tracheostomy tube, including its length and diameter, adapt. Therefore, also several length variants are available.


The Obturators
The standard length Tracoe Silcosoft tubes include a practical ring-shaped obturator. The ring-shaped grip allows intuitive handling of the obturator for the tube insertion which is particularly useful in smaller tube sizes.
The Tracoe Silcosoft proximally longer tubes and length variants include a metal obturator that is easily identifiable by the orange cap with clear marking for orientation.
Color Coding
Standard and proximal longer tubes are identified by blue printing on the neck flange with length and diameter variances. Length variants are identified with green printed information.
Do you want to know more about Tracoe Silcosoft?
Please fill out the form below, and we will get back to you shortly.
*verplichte velden
Deze site wordt beschermd door reCAPTCHA en het Privacybeleid en de Servicevoorwaarden van Google zijn van toepassing.
References
1 Edwards L, McRae J. Transitions in tracheostomy care: from childhood to adulthood. Current Opinion in Otolaryngology & Head and Neck Surgery. 2023; 10-1097.
2 Nakarada-Kordic I, Patterson N, Wrapson J, Reay SD. A systematic review of patient and caregiver experiences with a tracheostomy. Patient. 2018 Apr;11(2):175-191.
3 Watters K. Tracheostomy in infants and children. Pediatric tracheostomy. Respiratory Care. 2017; Vol. 62(6):803.
4 Fuller C, Wineland AM, Richter GT. Update on pediatric tracheostomy: indications, technique, education, and decannulation. Current Otorhinolaryngology Reports. 2021; 9:188-199.
5 Okonkwo I, Cochrane L, Fernandez E. Perioperative management of a child with a tracheostomy. BJA education. 2020; 20(1):18.
6 Tweedie DJ, Cooke J, Stephenson KA, Gupta SL, Pepper CM, Elloy MD, et al. Paediatric tracheostomy tubes: recent developments and our current practice. The Journal of Laryngology & Otology. 2018; 132(11):961-968.
7 Muller RG, Mamidala MP, Smith SH, Smith A, Sheyn A. Incidence, Epidemiology, and Outcomes of Pediatric Tracheostomy in the United States from 2000 to 2012. Otolaryngology–Head and Neck Surgery. 2019; 160(2):332-338.
8 Canning J, Mills N, Mahadevan M. Pediatric tracheostomy decannulation: When can decannulation be performed safely outside of the intensive care setting? A 10 year review from a single tertiary otolaryngology service. Int J Pediatr Otorhinolaryngol. 2020 Jun;133:109986.
9 Flanagan F, Healy F. Tracheostomy decision making: From placement to decannulation. Semin Fetal Neonatal Med. 2019 Oct;24(5):101037.
10 Gursoy TR, Eyuboglu TS, Aslan AT, Pekcan S, Buyukkaya EZ, Hangul M, et al. The associations between the clinical course of children with tracheostomy and their mothers’ depression, burnout, burden, and self-esteem. Journal of Clinical Nursing. 2023; 32(13-14):3412-3420.
11 Hall N, Rousseau N, Hamilton DW, Simpson AJ, Powell S, Brodlie M, et al. Providing care for children with tracheostomies: a qualitative interview study with parents and health professionals. BMJ open. 2023; 13(1):e065698.
12 Flynn A, Whittaker K, Donne AJ, Bray L, Carter B. Feeling stretched: parents’ narratives about challenges to resilience when their child has a tracheostomy. Journal of Child Health Care. 2023; 13674935231169409.
13 Pullens B, Streppel M. Swallowing problems in children with a tracheostomy. In Seminars in Pediatric Surgery. WB Saunders. 2021 June; 30(3):151053.
14 DeMauro SB, D’Agostino JA, Bann C, Bernbaum J, Gerdes M, Bell EF, et al. & Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Developmental outcomes of very preterm infants with tracheostomies. The Journal of pediatrics. 2014; 164(6):1303-1310.
15 Hess DR. Facilitating speech in the patient with a tracheostomy. Respiratory Care. 2005; 50(4):519–525.
16 Kraemer R, Plante E, Green GE. Changes in speech and language development of a young child after decannulation. Journal of communication disorders. 2005; 38(5):349-358.
17 Jiang D, Morrison GAJ. The influence of long-term tracheostomy on speech and language development in children. International journal of pediatric otorhinolaryngology. 2003; 67:S217-S220.
18 Sinha SK. The Respiratory System: Development and Physiology in the Neonate. In Clinical Anesthesia for the Newborn and the Neonate. Singapore: Springer Nature Singapore. 2023; 205-224.
19 Torres A, Cilloniz C, Niederman MS, et al. Pneumonia. Nat Rev Dis Primers. 2021; 7(25).
20 Powell J, Powell S, Mather MW, et al. Tracheostomy in children is associated with neutrophilic airway inflammation. Thorax. 2023; 78:1019-1027.
21 Morrison JM, Hassan A, Kysh L, Dudas RA, Russell CJ. Diagnosis, management, and outcomes of pediatric tracheostomy-associated infections: A scoping review. Pediatric pulmonology. 2022; 57(5):1145-1156.
22 Gipsman A, Prero M, Toltzis P, Craven D. Tracheobronchitis in children with tracheostomy tubes: Overview of a challenging problem. Pediatric Pulmonology. 2022; 57(4):814-821.
23 Zhu H, Das P, Roberson DW, Jang J, Skinner ML, Paine M, et al. Hospitalizations in Children with Preexisting Tracheostomy: A National Perspective. The Laryngoscope. 2014
24 Tan CY, Chiu NC, Lee KS, Chi H, Huang FY, Huang DTN, et al. Respiratory tract infections in children with tracheostomy. Journal of Microbiology, Immunology and Infection. 2020; 53(2):315-320.
25 Volsko TA, Parker SW, Deakins K, Walsh BK, Fedor KL, Valika T, et al. AARC Clinical Practice Guideline: management of pediatric patients with tracheostomy in the acute care setting. Respiratory care. 2021; 66(1):144-155.
26 Cline JM, Woods CR, Ervin SE, Rubin BK, Kirse DJ. Surveillance tracheal aspirate cultures do not reliably predict bacteria cultured at the time of an acute respiratory infection in children with tracheostomy tubes. Chest. 2012; 141(3):625-631.
27 de Kleijn BJ, van As-Brooks CJ, Wedman J, van der Laan BFAM. Clinical feasibility study of protrach dualcare a new speaking valve with heat and moisture exchanger for tracheotomized patients. Laryngoscope Investig Otolaryngol. 2017 Nov 27;2(6):453-458.
28 Vitacca M, Clini E, Foglio K, Scalvini S, Marangoni S, Quadri A, Ambrosino N. Hygroscopic condenser humidifiers in chronically tracheostomized patients who breathe spontaneously. Eur Respir J. 1994 Nov;7(11):2026-32.
29 Nelson Laboratories. Bacterial Filtration Efficiency (BFE) GLP Report. Salt Lake City, USA. Available on request from Atos Medical.
30 Nelson Laboratories. Viral Filtration Efficiency (VFE) GLP Report. Salt Lake City, USA. Available on request from Atos Medical.
31 Hess DR, Altobelli NP. Tracheostomy TubesDiscussion. Respiratory Care. 2014; 59(6):956- 973.
32 RP1, Myers C, Rutter MJ, et al. Prevention of tracheostomy-related pressure ulcers in children. Pediatrics. 2012; 129(3):e792-7.
MC3228-TcEN 202403
Delen